![]()
Vitamin B3
(Niacin a.k.a. Nicotinic acid)
The vitamin that prevents pellagra
![]()
![]()
Molecule of the Month January 2019
Also available: JSMol version.
![]()
Vitamin B3
|
 |
 It’s a disease that’s rarely heard of nowadays, but only a hundred or so years ago was responsible for thousands of deaths, notably in Europe and the Southern States of the USA. It actually gets its name from pell (holly-like) and agra (skin) in the Lombard language of Northern Italy, where the disease was endemic in the mid-1800s. It is a rather unusual disease, in that before about 1700 there were no historical mentions of it, but then it suddenly appeared and spread, until in the late 1800s, early 1900s it had reached epidemic proportions in the US Deep South. It’s estimated that between 1906 and 1940 more than 3 million Americans suffered from pellagra, with more than 100,000 deaths. In South Carolina alone, the number of deaths from this disease was 1,306 during the first ten months of 1915, and it was reported to have a nearly 40% fatality rate.
It’s a disease that’s rarely heard of nowadays, but only a hundred or so years ago was responsible for thousands of deaths, notably in Europe and the Southern States of the USA. It actually gets its name from pell (holly-like) and agra (skin) in the Lombard language of Northern Italy, where the disease was endemic in the mid-1800s. It is a rather unusual disease, in that before about 1700 there were no historical mentions of it, but then it suddenly appeared and spread, until in the late 1800s, early 1900s it had reached epidemic proportions in the US Deep South. It’s estimated that between 1906 and 1940 more than 3 million Americans suffered from pellagra, with more than 100,000 deaths. In South Carolina alone, the number of deaths from this disease was 1,306 during the first ten months of 1915, and it was reported to have a nearly 40% fatality rate.
Pellagra often appeared every year in Spring in the poorer States of the US South, after the meat-heavy diets eaten in the winter were replaced by corn, and so it became known as ‘Spring sickness’. The novel Hold Autumn in our Hand (George Sessions Perry, 1941) features Spring sickness as a major plot point in the story of a poor Texan farm family – and this was adapted into a Hollywood movie in 1945 called The Southerner starring Zachary Scott.
 What are the symptoms?
What are the symptoms?They include the 4 ‘D’s – diarrhoea, dementia, dermatitis (which is particularly bad in direct sunlight) and ultimately death. It’s caused by a vitamin deficiency, vitamin B3 to be precise, but that wasn’t known back then, and so the cause and prevention of pellagra became an urgent scientific mystery.
Just like in any good whodunnit, the scientists followed the clues. The first clue was that pellagra was most common in hot tropical areas with high poverty. As a result, many doctors believed the disease arose due to either bad genetics, an airborne pathogen, or ‘miasma’ (foul air) coming from poor sanitary conditions. But the second clue made these causes seem unlikely – pellagra was common in people who obtained most of their food from maize (corn). This finding was baffling, because maize had been imported into the US, and into Europe from South America, where it was a staple food of the local tribes, and had been for hundreds of years. However, these tribes didn’t seem to suffer from pellagra.
Indeed. So, instead, scientists started to think that perhaps the problem was caused by a micro-organism, impurity or toxin that had somehow contaminated the maize - one that wasn’t present in the original South American variety. But tests could find no evidence of any of these.
 Even odder…
Even odder…Yes, to solve the puzzle, in 1915, an American doctor called Joseph Goldberger (photo, right) set out to study pellagra. He noticed that doctors and nurses who worked closely with pellagra patients did not themselves contract the disease – so it didn’t appear to be infectious. He believed there was a dietary cause, and performed experiments on the children in orphanages and patients in mental asylums, many of who were suffering from pellagra. He fed half the patients with a varied diet of fresh meat, vegetables, milk and eggs, while the other (unlucky) half received the normal diet of mostly maize. The orphans/patients on the varied diet all recovered rapidly, while those on the normal diet remained sick. He had proven the link between pellagra and diet!
To find that, he needed to do more experiments, this time on prisoners. He managed to induce pellagra in inmates that had previously been healthy by simply replacing their standard meals with a purely maize-based one. Understandably, these experiments proved controversial, but he had at least shown that it wasn’t something in the maize that was causing the sickness, but rather something that was missing from it. Despite these rather dubious (by today’s standards) human experiments, and the fact that US Southern leaders resented a Northerner claiming that pellagra was due to the region’s poverty, he was nominated 5 times for a Nobel prize, although never won one.
The story shifts to Casimir Funk, who was a Polish biochemist with a special interest in diseases caused by dietary deficiencies. He’d heard about the pioneering experiments by Dutchman Christiaan Eijkman who had reported that Indonesian villagers who ate brown rice were less susceptible to the disease beri beri than those who ate only white rice (see MOTM for Sept 2017 about Vitamin B1). The reason was that milling the brown rice removed the husks and kernels, along with an unknown essential ingredient essential for health. Funk managed to isolate this ingredient, which he called vitamine (from 'vital amine'). He devised a theory that there are a number of these dietary ingredients that are essential for health, and published this in his 1912 book ‘The Vitamines’. Lack of a 'vitamine' in the diet led to diseases such as beri beri (B1), scurvy (C), or rickets (D). Later it was found that not all the ‘vitamines’ were amines, and so the ‘e’ was dropped from the name. The further complication was that the ingredient Funk had isolated from brown rice husks, and which had been called vitamin B, was actually 4 different molecules, each with a separate biological function. So they were renamed vitamin B1, B2, B3, etc., and various research groups set out to find what each one did. The molecule that prevented beri beri turned out to be B1 (thiamine), the one that promoted cell growth was B2 (riboflavin), while the one that prevented pellagra was B3.
Not quite – it took until 1938 for the conclusive experiments proving vitamin B3 prevented pellagra, first with experiments on dogs (where pellagra is manifested as a black tongue), and later in humans. The systematic chemical name for vitamin B3 is nicotinic acid, but scientists wanted to avoid any links to nicotine, in case the general public might get the incorrect idea that vitamins contain nicotine, or worse, that cigarettes contain vitamins! The name niacin was chosen from nicotinic acid and vitamin.
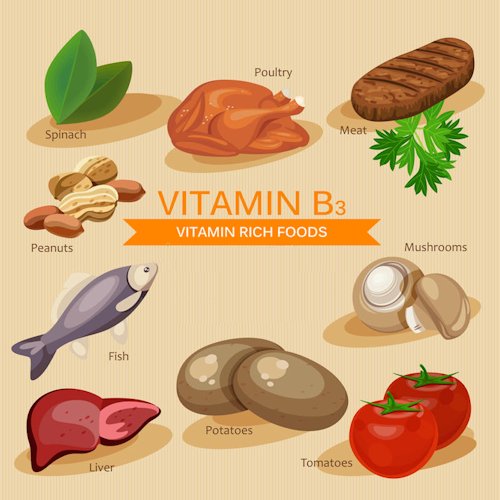
Foods rich in vitamin B3.
Once the solution was found, niacin was rapidly added to breakfast cereals and many other foodstuffs, so by the mid-1940s pellagra had almost disappeared from Europe and the US. Improved and more varied diets, especially increased consumption of meat and fish (such as tuna, pork and turkey) also helped, and nowadays pellagra is only ever seen in very deprived underdeveloped countries, warzones, or regions with extended poverty, malnutrition, or in patients with chronic alcoholism or anorexia. It is a triumph of modern science that in most developed countries, pellagra, the disease which caused so much suffering only a hundred years ago, is barely remembered.
But I still don’t understand why the original natives didn’t suffer from pellagra?This is a nice example of how mankind’s inventiveness can sometimes be surpassed by its arrogance. Remember the story of the brown rice, where milling it into the softer, more palatable white rice removed the husks containing the vital vitamin B1? Well, the story is similar here, except in reverse. The original maize grown by the South American Aztecs and Mayans was quite tough to mill, and so they used to boil it in lime (a strong alkali) for a couple of hours before milling. Amazingly, they had first developed this sophisticated chemical process (nowadays called nixtalamisation) nearly 2000 years ago. This process softened it and made it easier to mill. But, crucially, the strong alkali broke apart the hemicellulose scaffolding that was surrounding most of the corn cells, and released more of the niacin. This meant that the treated maize was effectively fortified in vitamin B3, so the natives did not get sick. |
 Left: Unprocessed, raw maize. Right: Nixtalamised maize. Photo: Ll1324, CC0 |
Maize was brought to Europe in 1498 by Christopher Columbus, and quickly spread through Europe, then to Africa and India. Early settlers then brought it to North America. However, Europeans had been processing tough grains for centuries and had developed various machines and technologies for removing the husks from grain that did not require the additional time-consuming and expensive nixtalamisation step. As a result, the milled but un-nixtalamised European (and later American) maize products were all very deficient in vitamin B3, although no-one realised this. Populations that ate this type of maize as their major (or only) source of nutrients were simply not getting sufficient vitamin B3 complex, which led to the pellagra epidemics.
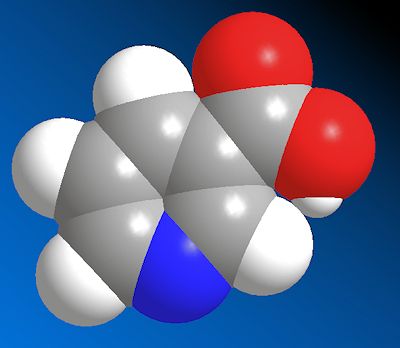
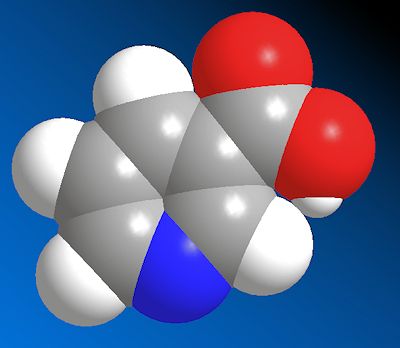
Because three related molecules actually make up what is commonly known as Vitamin B3, niacin, the amide derivative of this (nicotinamide), and nicotinamide riboside (which is nicotinamide with a ribose sugar group side group added to it). In the body the three (and possibly more) molecules are all interrelated by various biochemical processes, so it’s difficult to separate their effects.
 |
 |
| Niacin | Nicotinamide |
Both niacin and nicotinamide are precursors for two hugely important biochemical molecules. These are both coenzymes, which means they are helper molecules that allow enzymes to perform their function. The first of these is nicotinamide adenine dinucleotide (NAD), which is formed by joining two nucleosides (an organic molecule with a basic nitrogen atom, joined to a sugar) together via a phosphate link. The first one contains nicotinamide bonded to ribose and the other adenine bonded to ribose. Depending on the conditions inside the cell (e.g. the pH), NAD can exist in either the oxidised form with a positive charge (NAD+) or reduced form where a H is added (NADH).
The second coenzyme is the version of NAD with a phosphate group added to it, NADP (and its corresponding reduced version NADHP). The reduced form of both molecules can easily lose a H to form NAD+ or NADP+, respectively, with the ‘spare’ electron being donated to another molecule to oxidise it or to initiate a chemical reaction such as the loss of a hydrogen. NAD is involved in breaking down molecules, such as fats, sugars, proteins and alcohol, into smaller parts, while NADP does the reverse, it takes small molecules and builds them up into molecules such as fatty acids and cholesterol. As you might expect, with a deficiency of the precursors there would be less NAD and NADP, so that organs which have high energy requirements (e.g. the brain) or high renewal rates (such as the skin or gut), are the ones that exhibit the effects the most (remember the 4 ‘D’s?).
![]()
![]()
![]() Back to Molecule of the Month page. [DOI:10.6084/m9.figshare.5972449]
Back to Molecule of the Month page. [DOI:10.6084/m9.figshare.5972449]