|

Progesterone
The menstruation and pregnancy hormone

Sophie Goodall
University of Bristol

Molecule of the Month - December 2024
Also available: HTML version.

|

Progesterone - the pregnancy hormone
[Photo: Grant Source, CC BY 2.0 via Wikimedia Commons] |
Wait, don’t you mean Progestogen?
No, progestogens are a class of natural or synthetic hormones, with progesterone being the most important progestogen in the body. Progestogens play an important role maintaining pregnancy and being present at other stages of the menstrual cycle. The name is derived from the latin pro meaning ‘taking care of, supporting’ and gestāre or gestationem meaning ‘to bear, to carry’. Therefore, the progestogens heavily relate to fertility and the carrying of a foetus, and are required in all mammals for the survival and development of a baby.
So, it has something to do with sex?
Yes, in terms of reproduction. The sex hormones are important for sexuality and fertility. They are crucial as their release regulates sexual characteristics in both male and females once they hit puberty.
So progesterone is the sex hormone for females?
It is one of the sex hormones, however, it is not the only one. Progesterone belongs to one of three sex-hormone types, progestogens, the other two types being estrogens (a.k.a. oestrogens) including estradiol (the main female sex hormone (see MOTM page for July 2019), and androgens including testosterone (the main male sex hormone, see MOTM page for August 2019).
|

The end product of the reaction.
[Photo: Carin Araujo, Copyrighted free use, via Wikimedia Commons] |
What is its structure?
Progesterone is a white crystalline solid which is soluble in lipids and slightly soluble in water. The basic 4-ring steroid structure is also common for other sex hormones. Largely the structures are the same, however they vary in terms of their side groups. Progesterone has a 4-ring steroid structure with 21 carbons. There is a double-bond between the fourth and fifth carbon, and two ketone group. One is positioned at the third carbon and the other at the twentieth carbon.
 |
 |
 |
Estradiol
There are two OH groups present,
thus a ‘-diol’ suffix. |
Progesterone
There are two ketone groups and a double bond. Compared to estradiol,
the OH group has been oxidised, there is an additional methyl group,
the phenyl ring has been reduced and there are
two extra carbons on the five-membered ring. |
Testosterone
This has a remarkably similar structure to progesterone.
The notable difference is the loss of two carbons
and the addition of an OH group. |
|
|
|
How is it made in the body?
Progesterone is synthesised via the removal of a 6-carbon side-chain of the parent molecule cholesterol (see MOTM for March 2014) by use of an enzyme to make the molecule pregnenolone. The OH group is then oxidised to a keto group and the double bond moves from the fifth carbon to the fourth carbon. Progesterone is the end product in the ovary and placenta. However, in the adrenal cortex (the outer part of the adrenal gland) progesterone is used as an intermediate for the production of corticoids, androgens and oestrogens.
Conversion of cholesterol to progesterone.
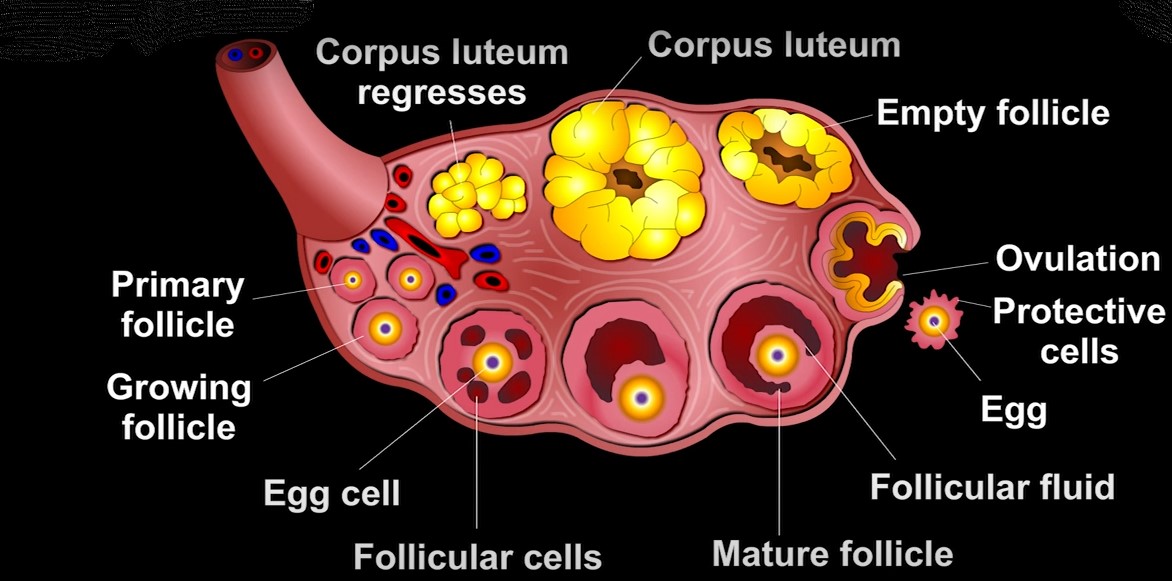
Progesterone can be produced by a variety of sources. To a small extent it is produced in nervous tissue such as the brain, and in fatty tissue. Small amounts are also produced by the largest part of the adrenal gland following the early stage of sexual maturation. But the main site for progesterone production is the corpus luteum - a temporary collection of cells that forms on the ovary each menstrual cycle whose purpose is to secrete a series of hormones that create an environment within the uterus suitable for pregnancy.
And one of those hormones is progesterone?
Yes, in fact, progesterone is essentially the main pregnancy hormone in females, as its IUPAC name might suggest: Pregnene dione (more accurately Pregn-4-ene-3,20-dione).
|
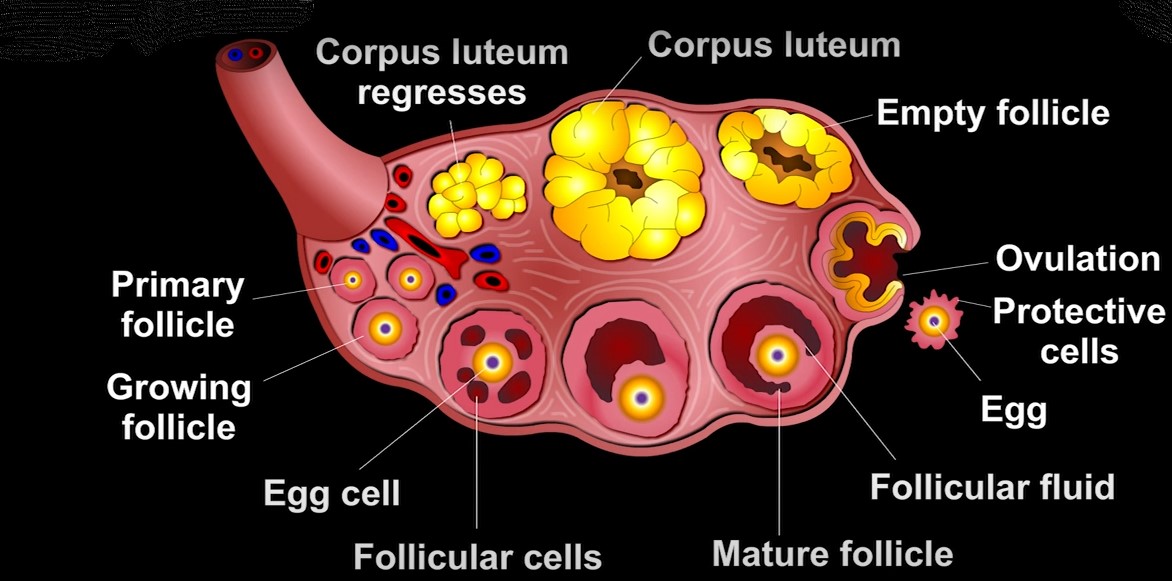
The various stages of development of the corpus luteum in an ovary.
[Image: Still image from You-tube video: What is
Corpus luteum? by Mercy Education Media. |
Really? So how?
Progesterone has a considerable role during the menstrual cycle. The cycle is divided into two consecutive phases, with each phase requiring a distinct set of hormones for the cycle’s development. During the cycle, around day 14, an egg is released from an ovarian sac called a follicle. The remains of these ovarian sacs, filled with fluid, form the corpus luteum, which releases progesterone during the second part of the menstrual cycle.
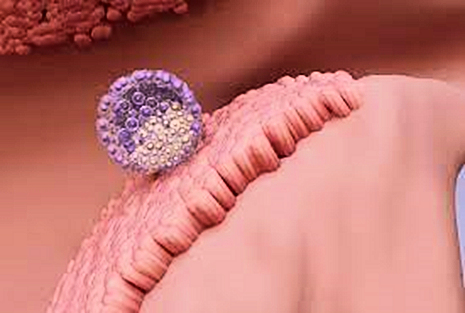
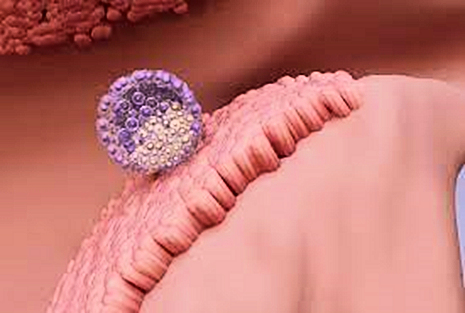
Implantation of an egg into the lining of the uterus
[Image: wistim.com] |
Once progesterone is released, it encourages the thickening of the uterine lining and then supports the early stages of pregnancy by creating a suitable environment for the fertilised egg to implant and grow. In the second phase of the cycle, progesterone levels in the blood increases to more than 3 ng/ml and this indicates that ovulation has happened. If implantation does not occur, meaning pregnancy does not happen, the production of progesterone will decrease, resulting in the uterine lining thinning and breaking down. This causes a menstrual bleed and thus a new menstrual cycle begins.
However, if implantation does occur, progesterone levels will remain heightened preventing the uterine lining from shedding. In the first trimester, the main production site for progesterone is the corpus luteum. However, this changes in the second and third trimester, where it is instead produced by the placenta. Progesterone stimulates the growth of blood vessels in the womb’s lining for increased blood flow and oxygen supply. In addition, progesterone also stimulates glands in the womb to release nutrients to the newly fertilised egg.
|
During pregnancy, progesterone levels increase gradually, until labour occurs. The total progesterone concentrations in the mother’s blood are typically 10 ng/ml in the first trimester and increases to 50 ng/ml then 100 ng/ml in the second and third trimester, respectively. Progesterone plays many key roles throughout pregnancy; strengthening the pelvic-wall muscles in preparation for labour, stimulating the growth of maternal breast tissue, and reducing the capability of the muscular wall of the uterus to contract. The decline in uterine contraction has the purpose of guaranteeing that implementation and development happen properly, while also discouraging premature removal of the developing baby.
So, does progesterone make women moody?
Well, moods are affected, yes. There are fluctuations of progesterone and other hormones during the menstrual cycle and these changes in hormone levels can impact the mood of women resulting in negative emotions, such as anger and irritability. Progesterone has an influence on a woman’s emotional processing, and is thought to be a cause for mood symptoms for those experiencing premenstrual syndrome (PMS). Following ovulation, blood progesterone levels rise and then decrease again before menstruation occurs. Too little progesterone, or the falling levels, have been suggested to be the cause of PMS.
In healthy women, the abilities to identify human emotions in others, and recalling memories which evoked emotions, are also influenced by progesterone levels. Identifying human emotions is worse when progesterone levels are higher, and there is a tendency to register negative stimuli more acutely, and to respond to them at a faster rate. This phenomenon has been explained as an adaptive heightened sensitivity toward physical threat as the body prepares for pregnancy. Moreover, when stressed, progesterone converts into the steroid hormone cortisol which increases responses to stress, another reason it may be the cause of menstrual-related mood symptoms.
|
[Photo by S.o.L.e on flickr] |
Can progesterone be synthesised in a lab?
Yes. Although progesterone is a naturally occurring hormone, there are synthetic forms of progesterone which are commercially produced by semi-synthesis. There are two main routes which are used to produce progesterone. The first method is the semi-synthesis from a plant steroid, developed by Marker in 1940, and the other from a stigmasterol, a plant sterol found in soybean oil.
 |
The Marker semi-synthesis
This reaction has six steps, which removes the spiroketal side-chain and converts it into the required side-chain to produce progesterone. The synthesis produces an intermediate by the name of 16-DPA which is important in this semi-synthesis and for the synthesis of many other medical steroids. |
 |
| The Soy semi-synthesis |
Why is it made synthetically, then?
It's used in the oral contraceptive pill. This became commercially available at the beginning of the 1960s, and gave women the ability to control their own fertility. The English magazine The Economist reported this form of contraception as ‘one the seven wonders of the modern world’ and ‘the one invention that historians a thousand years in the future will look back on and say: “That defined the 20th century”’.

The contraceptive pill
[Photo: Lupus in Saxonia, CC BY-SA 4.0 via Wikimedia Commons] |
Currently three different types of oral contraceptives are available to the public: combined oestrogen -progestogen (usually the oestrogen is ethinyl oestradiol), progesterone-only, and continuous or extended pill use. The combined pill with oestrogen and progesterone is the most prescribed hormone pill, where progesterone avoids pregnancy, and the oestrogen controls menstrual bleeding. When accurately taken, progesterone can alter the menstrual cycle by preventing the development of follicles and therefore stopping ovulation. The high levels of progesterone found in birth-control mirrors the levels in a woman’s body when pregnant. Therefore, the pill raises the hormone levels in the blood, tricking the body into thinking it has already conceived. The effects include no further ovulation; further eggs do not need to be released when the body believes one has already been fertilised. The pill can also make the fallopian tubes less likely to move the egg towards the uterus.
Another function of progesterone in contraceptive pills is to prevent sperm from penetrating through the cervix. It does this by thickening cervical mucus in the neck of the womb, creating a barrier that sperm cannot penetrate through. |
There are a variety of progesterone-only pills as well, and while the name can be deceptive, they contain only synthetic progestogens which are chemically related to progesterone, but are not the natural hormone itself. In the US, usual formulations contain the progestogens drospirenone or norethindrone. For this type of contraception, drospirenone inhibits ovulation, whereas norethindrone thickens cervical mucus, prevents ovulation, and adjusts the thickness of the uterine lining.
I suppose the 'pregnancy hormone' is found in women, right?
As a matter of fact, when it comes to progesterone secretion and progesterone blood concentrations, there is not a great quantitative difference between men and women. The levels found in males are close to those found in females in the first phase of the menstrual cycle. The adrenal glands and testes produce the hormone, and progesterone is essential for a male’s health and well-being, with men relying on the hormone to preserve masculinity. The hormone helps the male body to maintain lean muscle mass, regulate mood, and maintain a healthy prostate. In men, progesterone is involved in the synthesis of androgens, such as testosterone, as it is a testosterone precursor, and it can be converted to several other steroid hormones.
Progesterone also influences the final stage of sperm formation, and is thought to promote the reactions which lead to the maturation of sperm and subsequently the ability to fertilise an egg. Because progesterone is a precursor to testosterone and an prevents the action of estrogenic hormones, having a reduced level has implications on the male body. It can lead to a hormone imbalance, with too little testosterone and an increased level of estrogens. Inadequacy in progesterone levels can result in a phenomenon known as ‘oestrogen dominance’.
|

Progesterone helps the male body to maintain lean muscle mass,
as Senior Airman Terrence Ruffin demonstrated in 2015 on Eglin Air Force Base.
[Photo: US Air Force from USA, Public domain, via Wikimedia Commons]
|
[Image: Statisica.com, CC licence] |
Really, is that a bad thing?
Estrogen dominance is usually associated with women, where it isn't really a problem. However, in men it results in nervousness, erectile dysfunction, fatigue, higher risk of prostate cancer, prostate enlargement, and a low libido. Signs that a male has a significant increase in estrogen levels are visible through baldness, changes in body odour, breast growth, as well as reduced muscle development. Estrogen dominance can be especially worrying due to its impact on male reproductive health. This elevation in estrogen could damage male fertility because raised levels of estradiol (the most prominent estrogen) are thought to decrease testicular size and reduce the number of cells that go onto develop into sperm. Other studies have reported no sperm development for men with elevated estrogen. Therefore, a rise in male estrogen levels could lead to inadequate quantities and poor-quality sperm, meaning men could become infertile.
Indeed, global trends in sperm count had fallen on average by 1.2% per year between 1973 to 2018. Since 2000, there has been a steep decline in sperm count, with there being a decline at an accelerated rate of 2.64% per year as of 2017. While the factors responsible for this are yet to be clearly explained, an increase in estrogen is one possible reason for this trend. One of the most likely candidates is the accumulation of estrogenic molecules in lakes and rivers, often by people flushing unwanted or out-of-date birth-control pills down the toilet. There are also a number of industrial waste chemicals that cause biochemical side-effects very similar to those of estrogenic hormones, even though their chemical structure may be very different. Drinking water sourced from rivers and reservoirs polluted with these chemicals is a strong candidate for the declining fertility rates in men.
|
I’ve heard that low progesterone can lead to a miscarriage.
That's true. It has been reported the loss of progesterone during pregnancy is related to the rate of miscarriages and pre-term labour. One of the main functions of progesterone, as mentioned above, is to maintain a low level of blood vessels in the muscular outer layer of the uterus, meaning it is not capable of producing a contraction, and expelling the foetus as a result. The reduction in progesterone results in an increased blood flow, stronger muscles, and potentially an increase in the frequency and strength of these muscular contractions. These, together with simultaneous a decrease in protection against immunological threats, leads to a greater risk of miscarriage and premature labour.
If an embryo and pregnancy are healthy, inadequate progesterone production could result in a delayed development of the uterus’s inner lining at the time of implantation or during the beginning stages of pregnancy. The inadequate environment means the womb may not be ready to support the pregnancy and the baby won’t be carried to term. Therefore, infrequent, or recurring, miscarriages in the first trimester can occur. Studies have shown that taking progesterone supplements can reduce the risk of miscarriage, so hormone therapy when trying for a child can be helpful. This works as it increases the progesterone levels and may aid in the uterine lining thickening.
 Estimating miscarriages in early pregnancy can be difficult, because many women do not realise they are pregnant. The best estimate is that one-in-four pregnancies end in miscarriage. In addition, over 80% of these miscarriages happen in the first trimester.
Estimating miscarriages in early pregnancy can be difficult, because many women do not realise they are pregnant. The best estimate is that one-in-four pregnancies end in miscarriage. In addition, over 80% of these miscarriages happen in the first trimester.
What about abortion?
Interesting and nowadays, controversial, subject. Progesterone itself cannot be used to terminate an unwanted pregnancy as it is the pregnancy hormone. However, drugs that prevent the action of progesterone can be exploited to abort a foetus. The 'morning after pill', Mifepristone (see MOTM for March 2002, photo: right) is a drug which can cause abortion. In this case, it is taken orally to terminate a pregnancy and does so as it binds quicker and more strongly to progesterone receptors than the natural hormone does, inhibiting the normal response. This results in the structural breakdown of the uterine lining and the removal of an implanted fertilised egg.

Bibliography
Wikipedia: Progestogen, Progesterone;
- T. L. King, M. C. Brucker, in Pharmacology for Women's Health, ed. T. L. King, M. C. Brucker, Jones & Bartlett Learning, Burlington, Massachusetts, 1st edn, 2010, ch. 14, pp. 362-378.
- Cleveland Clinic, Progesterone, (accessed January 2024).
- Natracare, Are Hormone Names Sexist?,(accessed January 2024).
- Spencer TE, Bazer FW. Biology of progesterone action during pregnancy recognition and maintenance of pregnancy. Front Biosci. (2002) 7 d1879-98.
- H. Aliouche, An Overview Of Sex Hormones, News medical life sciences, (accessed January 2024).
- P.M Dewick, in Medicinal Natural Products: A Biosynthetic Approach, John Wiley & Sons Ltd, Chichester, 3rd edn, 2009, ch. 5, 187-310.
- D.F. Hawkins, M.G Elder, in Human Fertility Control, Butterworth-Heinemann, Oxford (UK), 1st edn, 1979, ch. 1, pp. 7-47.
- Cable JK, Grider MH. Physiology, Progesterone. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558960/
- C. Molnar, J. Gair, in Concepts of Biology, BCcampus, BC Open Textbook Project, 1st edn, 2015, ch. 24, pp. 1387 – 1461.
- J. Brynhildsen, Ther. Adv. Drug Saf.., (2014), 5(5), 201-213.
- The Economist, (1999), The Liberator, (accessed March 2024).
- Cooper DB, Patel P, Mahdy H. Oral Contraceptive Pills. [Updated 2022 Nov 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430882/
- M.L. Andersen, S. Tufik, Brain Research Reviews, (2006) 51(1), 136-143.
- M. Oettel, AK Mukhopadhyay, Taylor and Francis online, (2010) 7, 236-257.
- N.V. Goletiani, D.R. Keith, S.J. Gorsky, Exp. Clin. Psychopharmacol., (2007) 15, 427-444.
- M. Leavy, M. Trottmann, B. Liedl, S. Reese, C. Stief, B. Freitag, J. Baugh, G. Spagnoli, S. Kölle, Sci Rep., (2017) 7, 39931.
- , K. Latham, BBC news, (2023) Sperm quality appears to be declining around the world but is a little discussed cause of infertility. Now scientists are narrowing in on what might be behind the problem, (accessed March 2024).
- M. Hussain, S. El-Hakim, D. J. Cahill, J. Hum. Reprod. Sci., (2012) 5(3), 248-251.
- A. Beckley, (2021) Can low progesterone cause miscarriage?, (accessed February 2024).
- H.Y. Saglam, F. Basar, Pak. J. Med. Sci., (2019) 35(2), 515–520.
- O. Ford, A. Lethaby, H. Roberts and B. W. Mol, Cochrane Database of Systematic Reviews, (2012) 3(3) CD003415.
- I. Sundström-Poroma, E. Comasco, R. Summer, E. Luders, Front. Neuroendocrinol., (2020) 59, 100856.
- A.B. Handy, S.F. Greenfield, K.A. Yonkers, L.A. Payne, Harv. Rev. Psychiatry., (2022) 30(2), 100-117.
- B. M. Stifani, A.F. Lavelanet, BMJ, Sexual & Reproductive Health (2024) 50, 43-52.
- C. Czarnowsk, J. Bailey, S. Bal, Can. Fam. Physician, (2007) 53(9), 1531-1532.
- L. Martin (2024) Medical News Today, What are the symptoms of high estrogen?, (accessed February 2024)
- A.J. Ocampo, Health Gains, (2021) Progesterone for Men, (accessed February 2024)
- BodyLogicalMD, Learn How to Increase Progesterone in Men , (accessed February 2024)


 Back to Molecule of the Month page. [DOI:10.6084/m9.figshare.25860301]
Back to Molecule of the Month page. [DOI:10.6084/m9.figshare.25860301]
![]()
![]()
![]()
![]()




 Estimating miscarriages in early pregnancy can be difficult, because many women do not realise they are pregnant. The best estimate is that one-in-four pregnancies end in miscarriage. In addition, over 80% of these miscarriages happen in the first trimester.
Estimating miscarriages in early pregnancy can be difficult, because many women do not realise they are pregnant. The best estimate is that one-in-four pregnancies end in miscarriage. In addition, over 80% of these miscarriages happen in the first trimester.